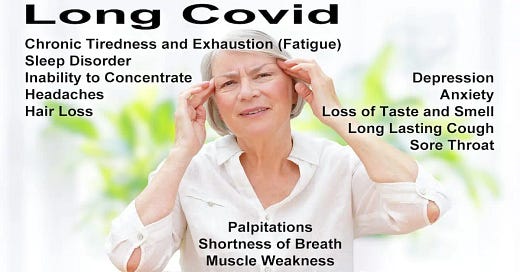
Long COVID Better Understood with Two New Research Articles
More research is good, but great treatments with data showing effectiveness still lacking
The first paper is a really interesting study conducted in the United Kingdom in which they tried to do a couple of things. One is they try to see whether there was an association of different long COVID symptoms and relate them to either people who were vaccinated or unvaccinated and the various variants of the COVID virus -- the wild type, the Alpha variant, and the Delta variant -- and they looked at the various symptoms in over 9,300 individuals.
They were able to identify three common patterns. There was a central neurologic cluster associated with the Alpha and Delta variants that caused things like brain fog and confusion.
There was a second cluster. It's called a cardiorespiratory cluster. It was typically linked to more severe symptoms, such as severe shortness of breath, cardiac issues, and lung problems associated primarily with the wild-type variant.
Then there was a systemic inflammatory cluster that often had immune-related symptoms. This transpired across all three different variants.
These clusters weren't affected by the vaccination status of the individual. It didn't appear to alter the profile or the type of long COVID symptoms associated with these different ones.
Here are the conclusions:
"We identified distinct self-reported symptom evolutions, or clusters, in individuals with more than 12 weeks of persisting symptoms after SARS CoV-2 infection, using a data-driven approach. Although multiple clusters were found across the three variants assessed, common features emerged for three clusters dominated by certain symptom groups: central neurological, cardiorespiratory, and systemic/inflammatory . Our findings may have relevance to individuals living with [long COVID], their health practitioners, and healthcare services, providing data to validate their illness and manage their expectations during its course. This work adds to the emerging evidence that PCS may have sub-types, possibly with differing pathophysiology. For any given individual, their condition may relate to a specific central/neurological process, to respiratory damage, or to a systemic inflammatory cause. Our study suggests that further investigation into mechanisms underlying [long COVID] should consider subdividing affected individuals into different subgroups, which may increase the ability to identify distinct processes underlying these symptom clusters."
The second paper looks at the risk of developing long COVID among quite a large cohort and establishes that as 1 in 8 will end up with these long COVID symptoms. It examined data from the US.
Here are stated results:
"The combined demographics of patients who attended long COVID clinics at the three N3C sites substantially differ from those of COVID-19 patients at these sites who did not attend a long COVID clinic (table). In this cohort, non-hospitalised long COVID clinic patients were disproportionately female. Long COVID clinic patients who were hospitalised with acute COVID-19 were disproportionately Black, when compared with all patients hospitalised with acute COVID-19, and were more likely to have a pre-COVID-19 comorbidity (diabetes, kidney disease, congestive heart failure, or pulmonary disease)."
"four themes emerged across the features and models: (1) post-COVID-19 respiratory symptoms and associated treatments, (2) non-respiratory symptoms widely reported as part of long COVID and associated treatments, (3) pre-existing risk factors for greater acute COVID severity, and (4) proxies for hospitalisation."
" review by clinical experts of the features [documented] revealed a number of possible themes."
"First, post-COVID-19 respiratory symptoms and associated treatments. These features are commonly reported for patients with long COVID.
A confounding factor that prioritises these features might be that the long COVID clinics at two of the three sites that contributed long COVID clinic patients are based in the pulmonary department. However, given that SARS-CoV-2 is primarily a respiratory virus, it is not surprising that long-term respiratory symptoms were observed. Similar long-term respiratory symptomatology is well described with respiratory viral syndromes, including those from severe acute respiratory syndrome, respiratory syncytial virus, influenza, and COVID-19.
The high proportion of albuterol use and use of inhaled steroids is consistent with the expected high prevalence of post-viral reactive airways disease. Examples of the most important features include dyspnoea or difficulty breathing, cough, albuterol, guaifenesin, and hypoxaemia.
Second, non-respiratory symptoms widely reported as part of long COVID and associated treatments. Sleep disorders, anxiety, malaise, chest pain, and constipation have all been reported as symptoms of long COVID, and are included in WHO's case definition.
The example features in this group include symptoms and mitigating treatments. Example features include dyssomnia, chest pain, and malaise, and treatments with lorazepam, melatonin, and polyethylene glycol.
Third, pre-existing risk factors for greater acute COVID severity. Some known risk factors for acute COVID-19 and severity are associated with long COVID—including chronic conditions (such as diabetes, chronic kidney disease, and chronic pulmonary disease), which predispose patients at increased risk for worsened COVID-19 symptoms.
Fourth, proxies for hospitalisation. Features that are representative of standard hospital admission orders probably contributed to the model as proxies for hospitalisation in general, rather than being individually meaningful. These features were most prominent in patients without long COVID (true negatives), suggesting that the model is correctly differentiating between acute illness requiring hospitalisation and long COVID. Example features include the use of glucose, ketorolac, propofol, and naloxone."
These two new studies caused The Washington Post to publish an editorial on August 15 titled "Long covid's long arm." For the second paper it noted that "post-covid symptoms lingered in about 1 in 8 people." It then went on to opine that "such a proportion could mean 70 million or more sufferers of long covid worldwide." But it also noted that other work has indicated a higher proportion of victims after infection, including work by CDC of a factor of 1 in 5 for adults age 18 to 64, and 1 in 4 for age 66 and over. Generally, most studies have indicated 20 to 30 percent hit by long COVID after infection.



Your analysis is sophisticated but there’s something to what I write here: https://robertyoho.substack.com/p/129-the-clot-shot-is-the-cause-of#details