Older Americans Greatly Harmed Despite High Vaccine Use
Risks persist for older people that COVID vaccines do not remove
The New York Times reported on high death rates in 2022. Here is what they said on May 31, 2022.
During the Omicron Wave, Death Rates Soared for Older People
Here are excepts:
Last year, people 65 and older died from Covid at lower rates than in previous waves. But with Omicron and waning immunity, death rates rose again.
Despite strong levels of vaccination among older people, Covid killed them at vastly higher rates during this winter’s Omicron wave than it did last year, preying on long delays since their last shots and the variant’s ability to skirt immune defenses.
This winter’s wave of deaths in older people belied the Omicron variant’s relative mildness. Almost as many Americans 65 and older died in four months of the Omicron surge as did in six months of the Delta wave, even though the Delta variant, for any one person, tended to cause more severe illness.
While overall per capita Covid death rates have fallen, older people still account for an overwhelming share of them.
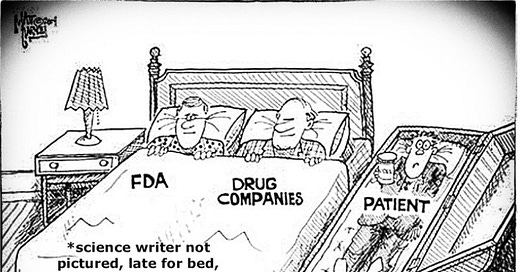
“This is not simply a pandemic of the unvaccinated,” said Andrew Stokes, an assistant professor in global health at Boston University who studies age patterns of Covid deaths. “There’s still exceptionally high risk among older adults, even those with primary vaccine series.”
Covid deaths, though always concentrated in older people, have in 2022 skewed toward older people more than they did at any point since vaccines became widely available.
As older people began dying at higher rates, Covid deaths also came to include higher proportions of vaccinated people. In March, about 40 percent of the people who died from Covid were vaccinated, according to an analysis of figures from the Centers for Disease Control and Prevention.
On the same day this article was published:
Long COVID in Older Adults: An Elusive Geriatric Syndrome
Here are excepts:
A recent report from the CDC said that nearly 60% of Americans, including 75% of children and adolescents, have been infected by SARS-CoV-2 as of February. As the virus continues to linger and mutate, that number will continue to rise, leading to higher rates of long COVID: a wide range of symptoms that can last more than 4 weeks or longer after the initial infection.
Issues like breathing difficulties, fatigue, high blood pressure, memory difficulties, mental health diagnoses (depression and anxiety), blood clotting, and kidney injury can now become a new, ongoing health battle -- possibly worse than the virus itself. Older Americans are once again left at high risk for potentially fatal complications.
In a recent study that included nearly 90,000 adults ages 65 and older who were diagnosed with SARS-CoV-2 infection, 32% reported symptoms of long COVID up to 4 months after infection. These striking findings imply that millions of older adults could be suffering from debilitating symptoms of long COVID. With these staggering numbers, and what we are seeing in our patients in hospitals and primary care facilities, we -- as clinicians -- need to reframe how we view and address long COVID in this population. We need to improve our approach to and management of long COVID.




When you aren't allowed to actually treat a disease, no surprise people get sicker and have long-term problems.